Implementing upper limb constraint induced movement therapy (CIMT) (face-to-face)



This workshop is run over 2 days and accepts 24 registrants.
This workshop enables small groups to work with clients and receive feedback from the presenters during clinical sessions.
Target audience: The workshop will be of interest to occupational therapists, physiotherapists and allied health assistants from hospital and community based settings, who provide upper limb rehabilitation to adults following stroke and acquired brain impairment, as well as university lecturers. The workshop focuses on upper limb rehabilitation.
Pre-reading and homework will be provided to the organising group for distribution to participants
This workshop focuses on helping therapists to minimise upper limb impairments post-stroke through the delivery of upper limb CIMT programs to eligible stroke survivors, and strategies to increase the delivery of this evidence based intervention in routine practice.
Course notes and content will be based on published research from both the CIMT and implementation science literature.
General Information
This face to face workshop provides an introduction to constraint induced movement therapy (CIMT) as an intervention for arm recovery after stroke and acquired brain injury and processes to support the implementation of CIMT into practice. Constraint-induced movement therapy (CIMT) is recommended in Australian (and other) stroke guidelines as an evidence-based therapy for arm recovery. Yet national audits show that only 12% of eligible Australian stroke survivors receive CIMT. Barriers to CIMT delivery include limited knowledge, skills, confidence, personnel and equipment. This workshop will enable professionals to develop their knowledge and skills in delivering a CIMT program and develop implementation strategies to support them to apply this knowledge to their practice.
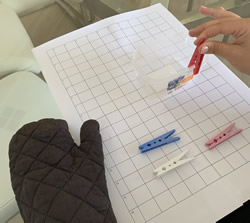
The workshop will describe what should be included in a CIMT program [beyond a mitt], how to structure and progress training during a CIMT program, how to measure participant change and overcome common barriers to delivering CIMT, particularly in public health settings. Video examples will be used to illustrate CIMT program components and opportunities provided to practice skills in assessment and delivery of components of a CIMT program with stroke survivor volunteers.
During the workshop, research will be presented and practical examples of evidence based implement strategies to support professionals and teams to run and sustain CIMT programs in routine practice.
Learning Objectives
By the end of the workshop, participants will be able to:
Identify
people that are eligible for CIMT
Name and describe
the key components of CIMT which include shaping, functional task practice, mitt wearing and a transfer package
Identify
the resources needed to deliver CIMT with fidelity including staff, space and equipment
Name
outcome measures that are commonly used before and after a CIMT program
Plan and conduct
an observational analysis and CIMT session (including shaping tasks, administration of the transfer package, coaching and feedback) with a person who has had a stroke
Identify
online educational resources that can be used to prepare for delivery of CIMT programs
Describe
the pros and cons of different models of CIMT delivery including 1:1, group and online/virtual
Presenters
Workshop Timetable
| Time | Day 1 |
|---|---|
| 8.00 | Introduction to workshop |
| 8.15 | What is CIMT? Evidence base including recent acute and telehealth updates.
Experiences of CIMT participants. |
| 9.10 | Deciding if a person is suitable for a CIMT program: Eligibility criteria. |
| 9.30 | Core component 1: Intensive graded practice using the affected upper limb part A Shaping
Ways to shape an activity. Interactive exercise: Task analysis and setting a shaping task. |
| 10.00 | Practical – Shaping exercise – video
The importance of accurately recording practice. |
| 10.30 | Morning Tea |
| 10.45 | Core component 1 Intensive graded practice using the affected upper limb part B Functional tasks – upgrading |
| 11.00 | Core Component 2: Mitt Wear |
| 11.20 | Core component 3: Transfer package: Considerations for home practice: use of adaptive equipment |
| 11.45 | Core component 3: Transfer package: Daily administration of MAL – video |
| 12.30 | Lunch |
| 1.15 | Prepare for practical session in small groups- review handover, gather up items you may need |
| 1.30 | Practical: Assessment of CIMT participant with goal setting, task analysis |
| 2.00 | Practical: Set up and run one shaping exercise |
| 3.00 | Practical: Establish home exercise program and mitt wear regime for overnight |
| 3.30 | Afternoon Tea |
| 3.45 | Debrief in small groups and Q and A |
| 4.30 | FINISH |
| Time | Day 2 |
|---|---|
| 8.00 | Interactive quiz – key concepts from day 1 |
| 8.30 | Models of CIMT delivery |
| 9.30 | Implementation activity: Designing a model of CIMT delivery for your service: Consideration of screening for eligibility, hours of therapy, hours of mitt wear, program duration, program frequency. |
| 10.45 | Morning Tea |
| 11.15 | Measuring change during a CIMT program: Upper limb assessment measures, COPM and use of video feedback |
| 11.45 | Implementation of CIMT programs in other public health services – Findings from the Australian Constraint Therapy Implementation study of the ARM (ACTIveARM) project and Q and A. |
| 12.45 | Lunch |
| 1.30 | Practical: Administration of the transfer package |
| 2.30 | Practical: Development of additional shaping exercises Development of functional task practice |
| 3.30 | Afternoon Tea including celebration of stroke survivor’s practice |
| 3.45 | Implementation activity: Designing a model of CIMT delivery for your service: Staffing mix, plans for education to patients and relatives, plans for long term sustainability e.g. supporting rotational staff. |
| 4.20 | Reflections on the day, workshop evaluation |
| 4.30 | FINISH |




